ALT Phalloplasty
Anterolateral Thigh Phalloplasty
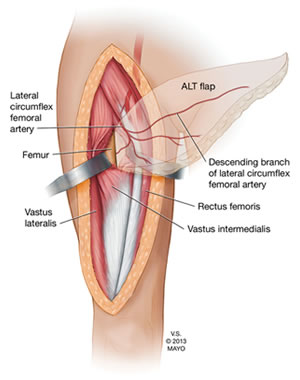
Anatomy of the ALT Flap. Source: Trans-vastus Intermedius Transfer of the Pedicled Anterolateral Thigh Flap for Posterior Thigh Reconstruction.
Anterolateral Thigh (ALT) Phalloplasty is a gender-affirming surgical technique that uses tissue from the thigh to create a penis that can be sensate, aesthetically natural, and functional for both sexual intercourse and urination while standing.
Table of Contents
- ALT Phalloplasty
- ALT Phalloplasty Variations
- Important Studies About ALT Phalloplasty
- Surgeons Who Offer ALT Phalloplasty
The ALT Flap
The ALT flap is composed of skin, fat, and fascia, with its blood supply provided by the descending branch of the lateral femoral circumflex vessels. Erogenous sensation is made possible by connecting the lateral femoral cutaneous nerve to one of the dorsal clitoral nerves. In some cases, an additional branch of the lateral femoral nerve can be connected to the ilioinguinal nerve to provide additional tactile sensation.
Donor Site Considerations
The ALT donor site is located on the outer thigh. This area can vary greatly in tissue thickness from patient to patient. In individuals with a thinner thigh, the flap may be ideal for both Stage 1 Urethroplasty and optimal aesthetic results. However, in patients with thicker subcutaneous fat, the bulk of the flap may:
- Preclude immediate urethral construction (Stage 1 Urethroplasty),
- Result in less desirable cosmetic outcomes, and/or
- Require staged debulking procedures and the use of secondary flaps like the SCIP flap for urethral reconstruction.
To determine candidacy for the ALT flap, The Pinch Test is commonly used to assess skin and subcutaneous fat thickness at the donor site. In addition, a preoperative multidetector CT scan (MDCT) is recommended to evaluate vascular anatomy and confirm the flap’s suitability for phalloplasty.
Urethral Reconstruction Options
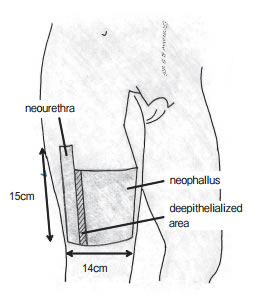
© 2013 by Okayama University Medical School
Urethroplasty with ALT Phalloplasty may be performed in different ways depending on patient anatomy and surgeon preference:
-
Complete Vascularized Urethroplasty using:
- “Tube-in-a-tube” using a segment of the ALT flap
- SCIP (groin) flap
- Labial or vaginal flaps
- Radial forearm flap (See Combined ALT/Forearm Phalloplasty)
-
Complete Non-vascularized Urethroplasty using:
- Buccal mucosa graft (higher risk of fistulas/strictures)
-
Partial Urethroplasty:
- Urethra is extended only to the base of the penis (lowest complication rate)
Surgical Staging
Staging for ALT Phalloplasty varies significantly depending on the surgeon and the patient’s healing process. A general timeline may include:
- Stage 1: Vaginectomy, phalloplasty, scrotoplasty
- Stage 1 or 2: Urethroplasty (sometimes split into Primary and Secondary Urethral Lengthening)
- Stage 1 or 2: Glansplasty (can be done 1 week after phalloplasty, but often delayed to stage 2)
- Stage 2 or 3: Testicular implant placement
- Final Stage: Erectile device implantation
Additional procedures, such as urethral revisions or cosmetic refinements, may be incorporated based on individual needs. On average, patients can expect a surgical and healing process that spans up to two years or longer, especially if complications arise.
Find out more about the various approaches to staging phalloplasty.
Hair Removal
Preoperative hair removal from the thigh is essential. Even with aggressive electrolysis and/or laser treatment beforehand, some individuals require additional hair removal after surgery, either due to urethral complications or aesthetics.
Learn more in our Patients' Guide to Pre-Operative Hair Removal for Phalloplasty.
Potential Complications
Like all phalloplasty techniques, ALT Phalloplasty carries potential risks. Early complications may include:
- Infection
- Bleeding
- Abnormal nerve sensations (paresthesia)
- Urethral fistulas or strictures
- Partial flap loss or necrosis
Some patients also experience leg weakness and adhesion formation (particularly with pedicled ALT flaps). Rare but severe complications include compartment syndrome and muscle necrosis.
Find out more about phalloplasty risks and complications.
Pros and Cons of ALT Phalloplasty
| Advantages | Disadvantages |
|---|---|
| Less obvious donor site, easily concealed with clothing | More challenging in patients with thicker skin and subcutaneous thigh fat |
| Shorter surgical time, especially with pedicled ALT | Excess girth can occur in some patients, requiring additional debulking |
| Good potential for sensation | Variable and less predictable blood vessel (perforator) anatomy complicates surgery |
| Suitable for urethroplasty in many patients | Sensation is generally less than with RFF phalloplasty (Monstrey et al., 2008) |
| Skin color typically matches well | Urethral complication rates may be higher compared to RFF phalloplasty (Ascha et al., 2017) |
ALT Phalloplasty Variations
Pedicled vs. Free Flap ALT Phalloplasty
Pedicled ALT Phalloplasty O.R. Video
Watch now »
The ALT flap can be used in both pedicled and free flap phalloplasty procedures. In the United States, pedicled ALT is more commonly performed.
In a pedicled flap, the tissue remains partially attached to the donor site through a “pedicle,” which continues to supply blood to the flap as it’s rotated or tunneled to the recipient site. Because the blood vessels are not completely severed, microsurgical connection is typically not required, though some surgeons may choose to connect additional veins to improve drainage. Avoiding microsurgery can reduce surgical costs and lower the risk of complications such as arterial clotting or flap loss.
In contrast, a free flap is completely detached from the donor site—along with its arteries and veins—and transferred to the recipient site. Blood flow is restored via microsurgical anastomosis, reconnecting the vessels. While technically more complex, this approach offers greater flexibility in flap positioning and can be beneficial for certain patients.
Learn more about flap types and how they differ from grafts on our Flaps & Grafts page.
Pedicled ALT Phalloplasty (sometimes referred to as “pALT”) preserves the flap’s native blood supply by keeping one end attached at the thigh. The flap is then rotated to the groin or pubic region. Microsurgical reconnection is usually not needed.
ALT Free Flap Phalloplasty fully detaches the flap from the thigh. Microsurgery is used to connect the arteries and veins to those at the recipient site to ensure blood flow.
“[Not performing microsurgery] avoids the low but real chance of a serious blood clot or other artery problem that can occur with RFF Phalloplasty. This problem usually requires emergency surgery to fix when it happens, so lowering the chance for this complication with ALT surgery increases the safety of the operation.”
— Dr. Richard Santucci
Delayed ALT Flap Phalloplasty
The Delayed ALT Flap technique is designed for patients who have a thicker thigh donor site, making them borderline candidates for ALT Phalloplasty, and who cannot or will not pursue radial forearm phalloplasty (RFF).
This method involves "delaying" the flap: a preliminary surgery is performed to partially interrupt the flap’s secondary blood supply while preserving its primary circulation. The flap is then left in place for 4–6 months, giving it time to strengthen and improve blood flow. After this delay period, the flap is used in phalloplasty surgery and transferred to the groin area to form the penis.
Although this technique adds an extra surgical stage, it provides critical benefits for certain patients:
- Enables use of the ALT donor site when it might not otherwise be viable
- Allows for controlled thinning of the flap over two surgeries
- Reduces risk of complications such as flap necrosis or lymphedema
This approach gives the flap time to stabilize and mature, improving blood flow and allowing careful sculpting before it's used to construct the penis and urethra.
Curious about how it works? Read the full surgical explanation.
Single Scar ALT Phalloplasty with Tissue Expansion
 Single Scar Phalloplasty (SSP) using tissue expansion is an emerging technique in gender-affirming surgery designed to minimize visible donor site scarring. This innovative method involves expanding a section of thigh skin prior to surgery so that the tissue can be harvested and the donor site closed with a single linear scar. Unlike traditional ALT phalloplasty that requires skin grafting and results in wide areas of scarring on the donor site, SSP allows for a more discreet aesthetic outcome. Currently, Dr. Dev Gurjala at Align Surgical in San Francisco is the only surgeon in the United States offering this technique. Learn more on our Single Scar Phalloplasty page.
Single Scar Phalloplasty (SSP) using tissue expansion is an emerging technique in gender-affirming surgery designed to minimize visible donor site scarring. This innovative method involves expanding a section of thigh skin prior to surgery so that the tissue can be harvested and the donor site closed with a single linear scar. Unlike traditional ALT phalloplasty that requires skin grafting and results in wide areas of scarring on the donor site, SSP allows for a more discreet aesthetic outcome. Currently, Dr. Dev Gurjala at Align Surgical in San Francisco is the only surgeon in the United States offering this technique. Learn more on our Single Scar Phalloplasty page.
Combined ALT/Forearm Phalloplasty
Combined ALT/Forearm Phalloplasty is a variant of the ALT procedure that uses a pedicled thigh flap to create the phallus, plus a small forearm graft to construct the neo-urethra. Using composite flaps increases the risk of complications, but for some patients, the trade-off is worth it to achieve specific functional or aesthetic goals. Learn more on our Combined ALT/RFF page.
Important Studies About ALT Phalloplasty
Dual Innervation in Anterolateral Thigh (ALT) Phalloplasty: Consider the Femoral Perforating Nerves [FULL TEXT]
Blair Peters et al., 2022
While ALT phalloplasty offers many benefits, one drawback has been that sensation in the penis is often not as strong or reliable as with the radial forearm flap technique. Surgeons typically connect only one nerve during ALT Phalloplasty—the lateral femoral cutaneous nerve. This study highlights another opportunity: the femoral perforating nerves, which are small nerves located along the inside edge of the thigh flap. These nerves naturally supply sensation to the area of the thigh that becomes the underside of the new penis—an area where sensation is especially important. By also connecting these femoral perforating nerves during surgery, patients could potentially experience better or more complete sensation. This technique, known as dual innervation, may help improve sensory outcomes.
Planned and Unplanned Delayed ALT Flap Phalloplasty [FULL TEXT]
Richard A. Santucci et al., 2021
Sometimes, the blood flow to the tissue used in ALT phalloplasty isn’t enough, which can cause healing problems. A technique called “vascular delay” helps improve blood flow by gently restricting some vessels before the main surgery, allowing new blood vessels to grow. This study found that using a delayed ALT flap approach doesn’t increase complications compared to the standard single-stage surgery. This means delaying the flap might be a safe option to reduce risks of partial flap loss and other problems.
Urethral Reconstruction in ALT Flap Phalloplasty: A 93-Case Experience
D’Arpa et al., 2019
This study looked at how often urethral problems happen after different types of ALT phalloplasty, like fistulas (leaks) or strictures (narrowing). They found that the “tube-in-tube” ALT technique had about a 20% complication rate, while some other methods had higher rates. Since the “tube-in-tube” method isn’t possible for most patients, surgeons often use other skin flaps (from the forearm or groin area) to build the new urethra. With these methods, about 92% of patients were eventually able to urinate standing up, which is a great outcome.
 The Pedicled Anterolateral Thigh Phalloplasty [FULL TEXT]
The Pedicled Anterolateral Thigh Phalloplasty [FULL TEXT]
Kyle Xu and Andrew Watt, 2018
The ALT flap offers a less noticeable donor site and good options for customizing penis size. However, compared to the radial forearm flap, it tends to have a higher chance of complications, especially involving the flap itself and the urethra. While the ALT can achieve key goals like standing urination, sexual intercourse, and a natural look, it often requires multiple surgeries and revisions. Choosing the right patients carefully is very important to get the best results.
More ALT Phalloplasty Journal Articles »
Surgeons Who Offer ALT Phalloplasty
- Dr. Rachel Bluebond-Langner & Dr. Lee Zhao - New York, US
- Dr. Bauback Safa, Dr. Andrew Watt & Dr. Mang Chen - Buncke Clinic / San Francisco Transgender Institute, California
- Dr. Dev Gurjala (Single Scar Phalloplasty) - Align Surgical, San Francisco, California
- Dr. Michael Safir - Align Surgical, Santa Monica, California
- Dr. Ellie Zara Ley - The Gender Confirmation Center, San Francisco, California
- Dr. Min Jun - Jun Surgical, San Francisco, California
- Dr. Loren Schechter - Rush University Medical Center, Chicago, Illinois
- Dr. Jonathan Keith - East Coast Advanced Plastic Surgery, Livingston, New Jersey
- Dr. Drew Marano - East Coast Advanced Plastic Surgery, New York, New York
- Dr. Gabriel Del Corral - MedStar Center for Gender Affirmation, Baltimore & Washington DC
- Dr. Daniel Freet - University of Iowa, Iowa City, Iowa
- Dr. Jens Berli & Dr. Blair Peters - OHSU, Portland, Oregon
- Dr. Kamol Pansritum (Combined ALT/Forearm Phalloplasty) - Thailand
Last updated: 06/22/25