Phallo.net » Risks and Complications
What is a Urethral Stricture?
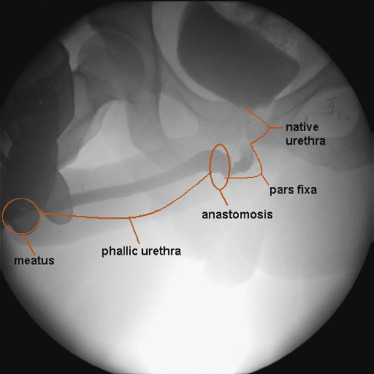 Urethral stricture is a narrowing or closure of the new urethra. The site of anastomosis between the fixed and phallic part of the urethra is the most common stricture location. This area is prone to fistulas and while these fistulas for the most part close spontaneously, they sometimes do so with excessive scarring, leading to stricture formation. Another explanation is that they form due to lower blood supply at the site of anastomosis, exacerbated by kinking at the base of the phallus. As a mucocutaneous junction this area is prone to stricture formation.1 Finally, hair growth in the urethra (from hair-bearing tissue used to construct the urethra) may play a role.
Urethral stricture is a narrowing or closure of the new urethra. The site of anastomosis between the fixed and phallic part of the urethra is the most common stricture location. This area is prone to fistulas and while these fistulas for the most part close spontaneously, they sometimes do so with excessive scarring, leading to stricture formation. Another explanation is that they form due to lower blood supply at the site of anastomosis, exacerbated by kinking at the base of the phallus. As a mucocutaneous junction this area is prone to stricture formation.1 Finally, hair growth in the urethra (from hair-bearing tissue used to construct the urethra) may play a role.
Strictures typically develop 6-12 months post-operatively. Symptoms include a weak urine stream and difficulty urinating. If surgical treatment is not pursued, the patient will likely face a lifetime of repeated manual dilations.2
Radial forearm free flap phalloplasty is associated with a rate of urethral stricture as high as 51%, which falls only to 23-35% even among the most experienced Phalloplasty surgeons.3
Treatment of a Urethral Stricture
Successfully treating urethral strictures in FTM Phalloplasty patients can be challenging for several reasons:4
- Absence of corpus spongiosum leads to poor coverage of any urethral reconstruction.
- Absence of foreskin, elastic penile skin, and scrotal skin makes reconstruction with preputial, penile, and scrotal skin grafts or flaps impossible.
- Wound-healing problems associated with phalloplasty can lead to dense local scar tissue.
 Reconstructive Urology is a sub-specialty of urology that focuses on restoring normal function in the urinary tract. A reconstructive urologist has the experience and specialized training necessary to treat complications arising from Phalloplasty surgery. Dr. Dmitriy Nikolavsky is Assistant Professor of Urology and Director of Reconstructive Urology at Upstate University Hospital in Syracuse, New York. Dr. Nikolavsky provides urological care for patients experiencing complications following Phalloplasty, such as urethral strictures.
Reconstructive Urology is a sub-specialty of urology that focuses on restoring normal function in the urinary tract. A reconstructive urologist has the experience and specialized training necessary to treat complications arising from Phalloplasty surgery. Dr. Dmitriy Nikolavsky is Assistant Professor of Urology and Director of Reconstructive Urology at Upstate University Hospital in Syracuse, New York. Dr. Nikolavsky provides urological care for patients experiencing complications following Phalloplasty, such as urethral strictures.
There are a number of different treatment options depending on the size and location of the stricture:5
- For short strictures near the tip of the penis, a small cut can be made to enlarge the opening of the urethra.
- For short strictures in the junction of the of the native and neo urethras, excision and closure of the stricture may be possible.
- For longer strictures in the junction of the of the native and neo urethras, or in cases where the above solution failed, excision and closure of the stricture augmented by buccal (inside of cheek) or bladder mucosa can be done in a single stage.
- For longer strictures in the shaft of the penis, or in cases where the above solution failed, excision and closure of the stricture augmented by buccal mucosa (inside of cheek)—or less commonly, remnants of vaginal mucosa, or rectal mucosa—can be done in in two stages, separated by 6 months.
- If difficult cases of persistent strictures, a final option is to relocate the urethra back to the perineum. Standing up to urinate without a device would not be possible.
The mean time between Phalloplasty and stricture repair surgery is almost 2 years, with a third of patients requiring more than one procedure.6 Lifetime urologic follow-up is recommended.7
WATCH: Dr. Michael Safir from the Crane Center discussing urinary strictures.
Prevention of a Urethral Stricture
Two stage Phalloplasty procedures generally have a lower rate of complications than single stage procedures, and pre-lamination with a full thickness graft can reduce the complication rate.8
"Patient and physician knowledge regarding the high burden and poor treatment options for urethral stricture after phalloplasty is incomplete, and patient acceptance of this reality is crucial for honest understanding of the potential complications of this increasingly common but extremely complex surgery." — Dr. Richard Santucci9
Read more about Phalloplasty Risks and Complications »
Footnotes
1. Lumen, Nicolaas et al. Urethroplasty for Strictures After Phallic Reconstruction: A Single-Institution Experience. European Urology , Volume 60 , Issue 1 , 150 - 158, http://www.europeanurology.com/article/S0302-2838(10)01083-3/fulltext#sec0010
2. Dmitriy Nikolavsky. "Urethral Stricture Disease", http://www.uroreconstruction.com/urethral-stricture-disease-2/.
3. Santucci, R. Review: Urethral Complications After Transgender Phalloplasty: Strategies to Treat Them and Minimize Their Occurrence. Clinical Anatomy, 2018 March, 31:187–190. https://onlinelibrary.wiley.com/doi/epdf/10.1002/ca.23021
4. Lumen, Nicolaas et al.
5. Dmitriy Nikolavsky et al, "Management of Unfavorable Urologic Sequelae After Phalloplasty in Transgender Patients," in Gender Affirmation: Medical and Surgical Perspectives (Thieme, Dec 1, 2016.)
6. Lumen, Nicolaas et al.
7. Monstrey SJ, Ceulemans P, Hoebeke P. Sex Reassignment Surgery in the Female-to-Male Transsexual. Seminars in Plastic Surgery. 2011;25(3):229-244. doi:10.1055/s-0031-1281493. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3312187/
8. Rashid M, Tamimy MS. Phalloplasty: The dream and the reality. Indian J Plast Surg [serial online] 2013 [cited 2017 Aug 2];46:283-93. http://www.ijps.org/text.asp?2013/46/2/283/118606
9. Santucci, R.
Last updated: 08/04/20