ALT Phalloplasty
© 2013 by Okayama University Medical School
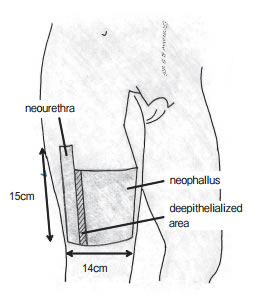
The ALT donor site is located on the thinner distal aspect of the thigh.
Anterolateral Thigh Phalloplasty
ALT Phalloplasty is a Phalloplasty procedure that uses the thigh donor site to create a sensate and aesthetically satisfactory penis that can be used for sexual intercourse and to urinate while standing.
The Anterolateral Thigh (ALT) Flap is a skin, fat and fascia flap that has blood supplied by the descending branch of the lateral femoral circumflex vessels. Innervation by provided by the lateral femoral cutaneous nerve which is connected to one of the dorsal clitoral nerves. An additional branch of the lateral femoral nerve can also be connected to the ilioinguinal nerve.
While the blood supply of the ALT flap is very good, the layout of the blood vessels can vary, making the surgery complex. The thickness of skin and sub-cutaneous fat of the thigh is also an important factor in determining if the ALT flap is indicated for Phalloplasty. Preoperative evaluation of the blood supply and subcutaneous fat via a multidetector CT scan (MDCT) is highly recommended.

"The Pinch Test" © Georg Thieme Verlag KG Stuttgart, New York.
In the right patient, the ALT flap can be quite thin, making it a good choice for sensation as well as Stage 1 Urethroplasty. Patients with thicker skin and more sub-cutaneous fat in the thigh may have excess tissue bulk in the ALT flap that can be a contraindication to Stage 1 Urethroplasty or may not provide aesthetically ideal results. For these patients, Urethroplasty and a debulking procedure can be performed at later stages. A secondary graft for Urethroplasty, such as SCIP flap, may also be indicated.
Urethroplasty can be approached in a few different ways:
- Complete Vascularized Urethroplasty: ALT flap segment, SCIP groin flap, labia & vaginal flaps, forearm flap
- Complete Non-vascularized Urethroplasty: buccal mucosa graft (higher rate of fistulas and strictures)
- Partial Urethroplasty: Urethra extended to base of penis only (lowest rate of complication)

© 2013 by Okayama University Medical School
The staging of surgeries with ALT Phalloplasty varies greatly depending on surgeon practices and patient healing, as well as logistics. Most patients can expect to have Vaginectomy, Phalloplasty and Scotoplasty at stage 1. Urethroplasty may be done at stage 1 or stage 2, or is sometimes split over two stages (Primary and Secondary Urethral Lengthening.) Glansplasty can be performed a week after stage 1 with ALT, but is also commonly delayed to stage 2. Implantation of testicular implants is done at stage 2 or 3, and erectile implant is done in the final stage. Urethral repair surgeries and/or cosmetic surgeries may also be incorporated into these stages. In general, one can expect to be fluctuating between surgery and healing stages for up to 2 years post-operatively, and longer if there are complications.
Removing hair from the ALT flap pre-operatively is required. Despite aggressive electrolysis and/or laser hair removal before surgery, some men require additional hair removal post-operatively, either for urethral issues or cosmetic reasons.
Potential complications early on in the post-operative period can include infection, bleeding, and paresthesia (abnormal sensation from damaged nerves); urethral issues such as fistula and stricture; and partial necrosis or flap loss. Some patients may experience leg weakness or develop adhesions (esp. with pedicled ALT.) Severe complications such as compartment syndrome and muscle necrosis are rare.
ALT Free Flap vs. Pedicled ALT Flap
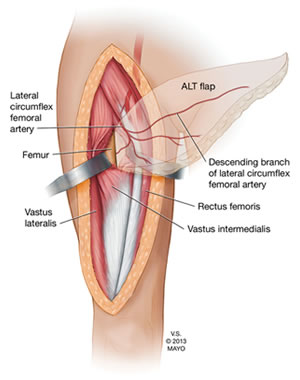
Anatomy of the ALT Flap. Source: Trans-vastus Intermedius Transfer of the Pedicled Anterolateral Thigh Flap for Posterior Thigh Reconstruction.
The ALT flap can be used for both free flap and pedicled Phalloplasty.
The term free flap refers to the "transplantation" of tissue from one site of the body to another. "Free" implies that the tissue, along with its blood supply, is completely detached from the original location ("donor site") and then transferred to another location ("recipient site") and the circulation in the tissue re-established by anastomosis of artery(s) and vein(s). This is in contrast to a "pedicled" flap in which the tissue is left partly attached to the donor site ("pedicle") and simply transposed to a new location; keeping the "pedicle" intact as a conduit to supply the tissue with blood. — Wikipedia
ALT Free Flap Phalloplasty uses an ALT flap that is completely detached from the donor site. Blood supply must be re-established by microsurgically connecting the arteries and veins of the flap and recipient site.
Pedicled ALT Phalloplasty (sometimes referred to as "pALT") uses an ALT flap that is left attached to the donor site at one end, while the other end is rotated to the recipient site, preserving blood supply. Microsurgical connection of blood supply is therefore not required, unless the surgeon chooses to hookup extra veins for drainage. Not performing this microsurgery lowers costs and more importantly, reduces the risks of blood clots and other arterial problems that can lead to necrosis and flap failure.
"[Not performing microsurgery] avoids the low but real chance of a serious blood clot or other artery problem that can occur with RFF Phalloplasty. This problem usually requires emergency surgery to fix when it happens, so lowering the chance for this complication with ALT surgery increases the safety of the operation." — Dr. Richard Santucci
Delayed ALT Flap
 The Delayed ALT Flap technique is offered by Dr. Curtis Crane. It's suited for patients with thick ALT flap donor sites who request ALT Phalloplasty and will not/cannot consider RFF Phalloplasty. It involves severing the secondary blood supply to the donor flap while preserving the main blood supply and leaving the flap in its original anatomical location. This gives the donor flap 4-6 months to adapt to the new blood supply before being moved to the groin area during Phalloplasty surgery. Delayed ALT Flap adds an additional stage to the surgery but allows patients who are borderline candidates for ALT, or who have blood supply issues in the ALT flap, to still use the ALT donor site.
The Delayed ALT Flap technique is offered by Dr. Curtis Crane. It's suited for patients with thick ALT flap donor sites who request ALT Phalloplasty and will not/cannot consider RFF Phalloplasty. It involves severing the secondary blood supply to the donor flap while preserving the main blood supply and leaving the flap in its original anatomical location. This gives the donor flap 4-6 months to adapt to the new blood supply before being moved to the groin area during Phalloplasty surgery. Delayed ALT Flap adds an additional stage to the surgery but allows patients who are borderline candidates for ALT, or who have blood supply issues in the ALT flap, to still use the ALT donor site.
"The surgery is staged, allowing for two opportunities to thin the flap while protecting the blood supply in the tissue to be used to make the neourethra and shaft. We perform a simultaneous subtotal vaginectomy and delay of the flap in the first stage. The flap is dissected in the usual fashion, except the tissue around its perforators is left unoperated. Fat deep to Scarpa's fascia is removed, which moderately reduces phallic girth. The superior incision line is not created at this time in order to decrease subsequent lymphedema of the flap. After 6 months, there is compensatory hypertrophy of the perforators, any tissue loss at the edge of the flap will have occurred and is discarded, and a second moderate thinning of the flap possible. We do not thin the flap during the typical single-stage ALT phalloplasty because of the increased risk of devascularizing the flap." — Carter EE, Crane CN, Santucci RA. Established and experimental techniques to improve phalloplasty outcomes/optimization of a hypercomplex surgery. Plast Aesthet Res 2020;7:33.
Combined ALT/Forearm Phalloplasty
Combined ALT/Forearm Phalloplasty is a variant of the ALT Phalloplasty procedure that uses a pedicled thigh donor flap to create the phallus, plus a small forearm graft to create the neo-urethra. Read more here.
Pedicled ALT Phalloplasty O.R. Video
Watch now »
Advantages of ALT Phalloplasty:
- Less obvious donor site, concealable with clothing;
- Decreased surgical time with Pedicled ALT;
- Good sensation;
- Good potential for urethroplasty;
- Good skin color match;
- Larger girth than RFF Phalloplasty;
- Some natural rigidity.
Disadvantages of ALT Phalloplasty:
- More difficult in patients with thicker skin and more subcutaneous thigh fat;
- In some patients, girth can be excessive;
- Less predictable perforator layout adds complexity;
- Sensation is reportedly less than RFF Phalloplasty (Monstrey et al., 2008);
- Reportedly higher urethral complication rate vs. RFF Phallplasty (Ascha et al., 2017).
Surgeons Who Offer ALT Phalloplasty
- Dr. Bauback Safa, Dr. Andrew Watt & Dr. Mang Chen - Buncke Clinic / San Francisco Transgender Institute, California
- Dr. Curtis Crane, Dr. Richard Santucci & Dr. Ashley DeLeon - Crane Center, Austin, Texas
- Dr. Kenan Celtik & Dr. Charles Lee - Crane Center, San Francisco, California
- Dr. Dev Gurjala (Single Scar Phalloplasty) - Align Surgical, San Francisco, California
- Dr. Michael Safir - Align Surgical, Santa Monica, California
- Dr. Ellie Zara Ley - The Gender Confirmation Center, San Francisco, California
- Dr. Min Jun - Jun Surgical, San Francisco, California
- Dr. Christopher McClung - Reconstructive Surgical Arts, Columbus, Ohio
- Dr. Loren Schechter - Rush University Medical Center, Chicago, Illinois
- Dr. Jonathan Keith - East Coast Advanced Plastic Surgery, Livingston, New Jersey
- Dr. Drew Marano - East Coast Advanced Plastic Surgery, New York, New York
- Dr. Gabriel Del Corral - MedStar Center for Gender Affirmation, Baltimore & Washington DC
- Dr. Daniel Freet - University of Iowa, Iowa City, Iowa
- Dr. Jens Berli & Dr. Blair Peters - OHSU, Portland, Oregon
- Dr. Narendra Kaushik - India
- Dr. Kamol Pansritum - Thailand - Combined ALT/Forearm Phalloplasty
- Dr. Rachel Bluebond-Langner - New York, US
- Dr. Christopher & Dr. Ralph - London, UK - Combined ALT/Forearm Phalloplasty
- Dr. Bouman & Dr. Buncamper - The Netherlands - ALT w/o Urethroplasty & Combined ALT/Forearm Phalloplasty
- Dr. Lundgren & Dr. Sigurjónsson - Sweden
- Dr. Stasevich - Belarus
- Dr. Rubino & Dr. Felici - Italy
- Dr. Chandra - India
- Dr. Pandey - India
Research
Planned and Unplanned Delayed Anterolateral Thigh Flap Phalloplasty
Richard A Santucci, Emma R Linder, Galen S Wachtman, Curtis N Crane. Plast Reconstr Surg Glob Open, 2021 Jun 22;9(6):e3654.
Pedicled anterolateral thigh (ALT) flap phalloplasty can be limited by inadequate perfusion. Vascular delay increases perfusion, as delay causes blood vessel formation by limiting the blood supply available to a flap before transfer. We hypothesized that delayed ALT flap phalloplasty would decrease rates of partial flap or phallus loss and other postoperative complications. Planned delay of ALT flaps provided similar results compared with those previously reported by our practice with standard single-stage approach.
Urethral Reconstruction in Anterolateral Thigh Flap Phalloplasty: A 93-Case Experience.
D'Arpa S, Claes K, Lumen N, Oieni S, Hoebeke P, Monstrey S. Plast Reconstr Surg. 2019 Feb;143(2):382e-392e.
Urethral complication rates (fistulas and strictures) were as follows: tube-in-tube anterolateral thigh flap, 20 percent; prelaminated anterolateral thigh flap, 87.5 percent; free radial forearm flap urethra, 37.9 percent; superficial circumflex iliac artery perforator urethral reconstruction, 26.3 percent; and skin flap from previous phalloplasty, 16.7 percent. When tube-in-tube urethra reconstruction is not possible (94.2 percent of cases), a skin flap such as the superficial circumflex iliac artery perforator flap or the radial forearm flap is used for urethral reconstruction in anterolateral thigh phalloplasties. Flap prelamination is a second choice that gives high stricture rates. If a penis is present, its skin should be used for urethral reconstruction and covered with an anterolateral thigh flap. With these techniques, 91.86 percent of patients are eventually able to void while standing.
The Pedicled Anterolateral Thigh Phalloplasty.
 Xu KY, Watt AJ. Clin Plast Surg. 2018 Jul;45(3):399-406.
Xu KY, Watt AJ. Clin Plast Surg. 2018 Jul;45(3):399-406.
The primary advantages of the ALT flap are the inconspicuous donor site and flexibility in phallus length. The disadvantages of the ALT flap are a higher incidence of both flap and urethral complications compared with a Radial Forearm Phalloplasty. Although ALT phalloplasty can achieve the primary goals of standing micturition, penetrative intercourse, and an aesthetic phallus, multiple stages and revisions are often necessary. Careful patient selection is paramount in attaining acceptable results.
More ALT Phalloplasty Journal Articles »
Last updated: 06/05/24