Phalloplasty Risks and Complications
The importance of educating patients about Phalloplasty risks and complications can't be overemphasized. While all surgeries come with risks, FTM Phalloplasty certainly qualifies as a high risk/reward procedure. Techniques have drastically improved since the surgery was first performed in 1946, reducing complication rates overall, but FTM Phalloplasty remains technically challenging. Nevertheless, a review of 29 academic studies revealed a remarkably high rate of satisfaction among Phalloplasty patients, and also showed that 95% of transsexual men are able to stand-to-void following Phalloplasty with Urethroplasty.
There are some important things to keep in mind when considering Phalloplasty risks and complications:
- Different surgical methods of Phalloplasty have varying levels of complexity and risks;
- Surgeons will likely have different complication rates;
- Complication rates may be self-stated by the surgeon or published in peer-reviewed academic journals. Self-stated statistics may be less accurate.
"I tell all my patients that the complication rate for Phalloplasty can be 100%. It could be a small opening, but it's 100%. There's something that's going to happen. The question is how do we as surgeons really try to navigate minimizing all the potential issues." — Dr. Gabriel Del Corral
General Risks of Surgery include: Infection, bleeding, damage to surrounding tissues, pain.
Common (and Not So Common) Phalloplasty Complications
 Urethral complications
Urethral complications
- Wound breakdown
- Pelvic bleeding or pain
- Bladder or rectal injury
- Lack of sensation
- Prolonged need for drainage
- Partial necrosis or flap loss
- Dissatisfaction with the size or shape of the penis
- Need for further procedures
Donor Site Risks
- Wound breakdown
- Decreased mobility
- Hematoma
- Pain
- Decreased sensation
- Excessive scarring
- Hypergranulation, slowing down wound healing and raising risk of infection.
- Adhesions: A band of scar tissue that binds two parts of tissue together.
Early On-Set Complications
Urethral complications are fairly common with Phalloplasty when urethral lengthening is performed. Urinary fistula is an opening in the urethra that causes urine leakage. Precise estimates of the risk of fistula are difficult to ascertain, but they can differ by procedure:1
- Suprapubic abdominal flaps have a high fistula rate of 55%.
- Radial Forearm Phalloplasty has reported fistula rates ranging from 22 to 68%.
- Prelaminated Osteocutaneous Fibula Flap Phalloplasty has fistula rates ranging from 15 to 22%.
- Surprisingly, the pedicled flaps namely the Anterolateral Thigh Flap and the extended pedicle groin flap had the lowest reported fistula rates of <10%. (In the ALT study referenced, the patients were cis gender.)
A more recent study published in July 20172 compared urethral complications in patients who had had either Radial Forearm (RFF) or Anterolateral Thigh (ALT) Flap Phalloplasties:
Overall urethral complication rate for RFFF phalloplasty was 31.5%; the overall pALT rate was 32.8%. The rate of partial or total neophallus loss was 7.8% for pALT and 3.4% for RFFF. Patients in the pALT cohort experienced significantly greater odds of urethral fistula (OR=2.50, p=0.024), non-urethral complications (OR=2.38, p=0.027), and phallus wound dehiscence (OR=5.03, p=0.026).
Other potential urinary complications in the early days following surgery can also include partial or total death of the tissue used to create the new urethra, a clogged catheter, bladder spasms and urinary tract infections (UTIs).
Wound infections can present as cellulitis, fungal infection or both. Antibiotics and antifungal cream are usually sufficient for treatment.
Wound breakdown commonly occurs at points where multiple incisions meet, such as the base of penis. Most wound breakdown complications can be treated with local wound care but more serious issues may require may require surgical intervention to close the wound.
Hematomas can occur and are usually managed by drains, though some may require surgical drainage.
Bladder and rectal injury are rare but serious complications. Inadvertent injury to the bladder or rectal wall can occur during the Vaginectomy that is performed during Phalloplasty. Early detection is critical as the injury can be repaired during surgery. If not, the patient may develop symptoms of sepsis and require surgical intervention. In some cases, multiple surgieries over a period of many months are required to treat bladder and rectal fistulas.
Partial necrosis and flap loss are fairly rare, with a rate of up to 18% 3, and typically present within the first 72 hours after surgery. Early detection and treatment is critical to salvaging the flap.
Long-term Complications
Urethral stricture is a narrowing or closure of the new urethra caused by scar tissue or hair growth in the urethra. Strictures typically develop 6-12 months post-operatively. Symptoms include a weak urine stream, difficulty urinating, or a complete inability to urinate. If surgical treatment is not pursued, the patient will likely face a lifetime of repeated dilations.4
Postvoid incontinence or dribbling occurs in about 79% of Phalloplasty patients according to this study. 5
Wound contracture leading to distortion of surrounding tissues and contour defects.
Scars can stretch, become red and raised (hypertrophic), or grow beyond their original dimensions (keloid).
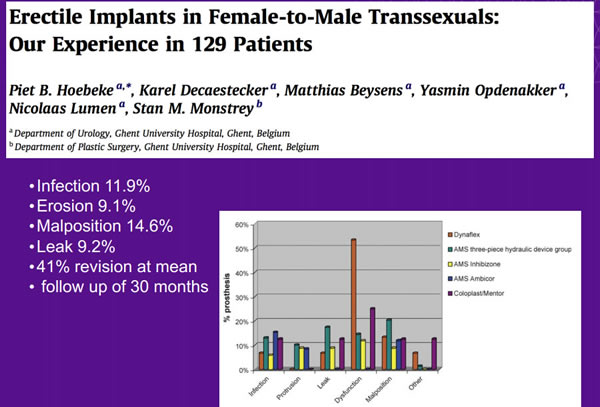
Risks Associated with Penile and Testicular Implants
Infection is the most common complication with implants. If an implant becomes infected, it typically has to be removed. Replacement can occur six months later.
Erosion is when the implant breaks through the skin. Surgical removal is required if this occurs.
Loss or displacement of testicular implants occurs at a rate of 2-30% and can increase the risk of urethral complications.6
If all this is starting to sound like doom and gloom, here's an upside: trans men undergoing Phalloplasty have a lower complication rate than cis gender men.7 Researchers from Norfolk, Virginia compared Phalloplasty outcomes via data analysis of transgender (53%) and non-transgender patients (47%) who underwent Phalloplasty at their institution between 1983 and 2015. Results from the comparison showed that those in the transgender group had a lower rate of post-operative complications compared to those in the non-transgender group (45 percent vs. 63 percent, respectively). The flipside? Transgender patients also demonstrated a statistically significant increased rate for urethral strictures compared to non-transgender patients (56 percent vs. 30 percent, respectively).
UPDATE, OCT 2017
Outcomes After Phalloplasty: Do Transgender Patients and Multiple Urethral Procedures Carry a Higher Rate of Complication? This large review study 8 concluded that cismale patients undergoing phalloplasty had lower urethral and flap complication rates compared to transmale patients. Primary urethroplasty had superior outcomes of voiding while standing, sexual function, and patient satisfaction compared to staged urethroplasty, which had more flap complications. However, in many of the studies included in the review urethroplasty was performed prior to the development of tube-in-tube design or in flaps that did not accommodate a single staged urethroplasty.While the list of risks and potential complications with Phalloplasty is daunting, several studies have revealed high satisfaction rates among trans men. When complications arise, they can most often be managed by the original surgeon or by a Reconstructive Urologist or Plastic Surgeon experienced with Phalloplasty complications and repair surgeries.
Footnotes
1. Rashid M, Tamimy MS. Phalloplasty: The dream and the reality. Indian J Plast Surg [serial online] 2013 [cited 2017 Aug 2];46:283-93. http://www.ijps.org/text.asp?2013/46/2/283/1186062. Ascha M, Massie JP, Morrison SD, Crane CN, Chen ML. Outcomes of Single-Staged Phalloplasty by Pedicled Anterolateral Thigh Flap versus Radial Forearm Free Flap in Gender-Confirming Surgery. J Urol. 2017 Jul 29.
3. Lynne Carroll, Lauren Mizock. Clinical Issues and Affirmative Treatment with Transgender Clients. Elsevier Health Sciences, Feb 7, 2017.
4. Dmitriy Nikolavsky. "Urethral Stricture Disease", http://www.uroreconstruction.com/urethral-stricture-disease-2/.
5. Hoebeke P, Selvaggi G, Ceulemans P, De Cuypere G, T'Sjoen G, Weyers S, Decaestecker K, Monstrey S.Impact of sex reassignment surgery on lower urinary tract function. Eur Urol. 2005 Mar;47(3):398-402. Epub 2004 Dec 2. https://www.ncbi.nlm.nih.gov/pubmed/15716207
6. Selvaggi G, Hoebeke P, Ceulemans P, Hamdi M, Van Landuyt K, Blondeel P, De Cuypere G, Monstrey S. Scrotal reconstruction in female-to-male transsexuals: a novel scrotoplasty. Plast Reconstr Surg. 2009 Jun;123(6):1710-8. http://www.ncbi.nlm.nih.gov/pubmed/19483569
7. Oscar Suarez Fernandez De Lara, Jack M. Zuckerman, Ramon Virasoro, Jeremy Tonkin, Jessica Delong, Kurt A. McCammon. Difference In Outcomes After Total Phallic Reconstruction In the Transgender and Non-Transgender Population. The Journal of Urology, Volume 195, Issue 4, e790 (April 2016)
8. Remington AC, Morrison SD, Massie JP, Crowe CS, Shakir A, Wilson SC, Vyas KS, Lee GK, Friedrich JB. Outcomes After Phalloplasty: Do Transgender Patients and Multiple Urethral Procedures Carry a Higher Rate of Complication?
Plast Reconstr Surg. 2017 Oct 10.
Last updated: 11/16/21