Flaps & Grafts: What’s the Difference?
Phalloplasty comes with a lot of unfamiliar terminology. Understanding these terms can help you feel more informed, communicate more clearly with your surgeon, and approach your surgery with greater confidence. One of the most important distinctions in terminology is the difference between flaps and grafts.
In this article, we’ll break down what flaps and grafts are, how they’re used in phalloplasty, and why understanding the difference can empower you in planning your surgery. We’ll also take a closer look at different types of skin grafts, as well as the differences between split-thickness and full-thickness skin grafts.
What Are Flaps?
A flap is a section of tissue, usually including skin, fat, fascia, and sensory nerves, that’s taken from one part of the body and used to create the penis in phalloplasty. What makes a flap different from a graft is that it includes its own blood supply. In some cases, the tissue stays connected to its original blood vessels and is tunneled to the surgical site (this is called a pedicled flap). In other cases, the tissue is completely detached and the blood vessels are reconnected in the new location using microsurgery (this is called a free flap).
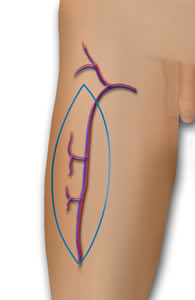
ALT Donor Site
Source: microsurgeon.org
The most well-known example of a flap in phalloplasty is the radial forearm flap (RFF), where the donor site is the forearm. The tissue is fully removed from this area and then reattached to blood vessels in the groin, making it a free flap. Another common donor site is the anterolateral thigh (ALT). The ALT flap is most often used as a pedicled flap, meaning the blood supply stays connected while the tissue is tunneled into place, but some surgeons use it as a free flap depending on the patient’s anatomy and surgical plan.
Some flaps also include muscle in addition to skin, fat, fascia and nerves. For example, the latissimus dorsi (MLD) flap is a myocutaneous flap, meaning it includes a portion of the latissimus dorsi muscle. The added muscle helps provide bulk and shape to the penis, especially in patients with limited subcutaneous fat. While including muscle can improve contour, it may also impact muscle function at the donor site. Most other common phalloplasty flaps which don't include muscle, such as the radial forearm and anterolateral thigh, are known as fasciocutaneous flaps.
Some other donor sites used in phalloplasty include areas where muscle is also taken. One example is the groin flap, which may include some muscle or connective tissue depending on the surgeon’s technique. Another is the gracilis flap, which uses the gracilis muscle from the inner thigh. Dr. Rachel Bluebond-Langner and Dr. Lee Zhao at NYU use this muscle in addition to RFF or ALT flaps to help rebuild parts of the urethra and fill in the vaginal space following vaginectomy. In this approach, the gracilis muscle is carefully moved through a tunnel from the groin area to the vaginal cavity. The muscle is then split into two parts: one part is placed inside the vaginal space, and the other part is wrapped around the new urethra to provide extra support and help it heal better with a good blood supply.
The choice of flap type depends on many factors, including body type, aesthetic and sensory goals, and the surgeon’s approach.
What Are Grafts?
Unlike flaps, which bring their own blood supply, grafts are pieces of skin that rely entirely on the new site (called the recipient bed) to provide blood flow and nutrients. Because they don’t come with their own blood vessels, grafts need careful handling and optimal healing conditions to successfully “take.”
In phalloplasty, grafts are most commonly used to cover flap donor sites, especially in procedures like radial forearm phalloplasty. They may also be used in urethral reconstruction, glansplasty, and other refinements where additional tissue is needed. Grafts don’t contain nerves, but they may regain some sensation over time through a slower and less predictable process called nerve ingrowth.
In some types of phalloplasty, grafts aren’t needed at all if the flap donor site can be fully closed with sutures. This is called primary closure and is often possible with flaps taken from areas like the abdomen or the latissimus dorsi (MLD), which usually have more available skin and tissue to allow for complete closure without needing a skin graft. Another example is Single Scar ALT phalloplasty, a newer technique designed to minimize visible scarring by aiming for primary closure at the donor site through the use of pre-operative tissue expansion. Whether grafts are needed depends on factors such as donor site size, patient body type, and the specific surgical technique used.
Comparing Grafts & Flaps in Phalloplasty
When deciding between flaps and grafts in phalloplasty, surgeons consider several important factors. Flaps, which bring their own blood supply, tend to heal more reliably and are often used for major structures like the penis itself because they provide better durability and sensation. Grafts, on the other hand, depend entirely on the new site’s blood flow and are generally thinner and less robust. This means grafts may be more prone to complications like partial loss (necrosis), or issues such as fistulas and strictures, especially when used inside the urethra. Because they’re thicker and more durable, flaps are generally better suited for creating the penis itself. Both techniques often work together to achieve the best functional and aesthetic results.
Split-Thickness vs. Full-Thickness Grafts
In phalloplasty, two main types of skin grafts are used: split-thickness and full-thickness. They differ in how much skin is taken and how they heal.
 Split-thickness grafts are the most common type used in U.S. phalloplasty surgeries, especially for RFF, ALT and urethral reconstruction. These grafts include the outer layer of skin (epidermis) and part of the dermis. Because they’re thinner, they’re easier for the body to support and heal. That’s why they’re widely used to cover large donor sites. However, because split-thickness grafts don’t include hair follicles, the grafted area won’t regrow hair. These grafts also tend to shrink more during healing and may not match the surrounding skin as naturally as full-thickness grafts. The graft donor site takes longer to heal and needs more wound care.
Split-thickness grafts are the most common type used in U.S. phalloplasty surgeries, especially for RFF, ALT and urethral reconstruction. These grafts include the outer layer of skin (epidermis) and part of the dermis. Because they’re thinner, they’re easier for the body to support and heal. That’s why they’re widely used to cover large donor sites. However, because split-thickness grafts don’t include hair follicles, the grafted area won’t regrow hair. These grafts also tend to shrink more during healing and may not match the surrounding skin as naturally as full-thickness grafts. The graft donor site takes longer to heal and needs more wound care.
Full-thickness grafts are less commonly used in the U.S. but are used in some international practices, like in the U.K. These grafts include both the epidermis and the full thickness of the dermis. Because they bring along hair follicles and tend to retain color, they can look and feel more like natural skin over time. The graft donor site can often be closed with stitches, leaving a scar similar to a tummy tuck or butt lift. There’s a higher risk of tissue loss though, since the graft is thicker and harder for the body to support. They’re better suited for smaller areas like the forearm (RFF), not the thigh (ALT), due to the risk of complications and wound size.
Flaps and grafts are essential building blocks of phalloplasty—they influence how the body heals, and how the skin looks and feels. Being informed about the differences between flaps and grafts can help you set realistic expectations, have meaningful conversations with your surgeon, and feel more confident about your recovery and long-term outcomes.
Glossary
| Term | Definition |
|---|---|
| Flap | A section of tissue (skin, fat, fascia, and sometimes muscle and nerves) moved to another part of the body with its own blood supply. |
| Graft | A piece of skin moved to a new location without its own blood supply; relies on the new site to survive. |
| Fascia | (Pronounced FAY-sha) A layer of connective tissue that surrounds and supports muscles, nerves, and blood vessels. |
| Free Flap | A flap that is completely detached from its original location and reattached using microsurgery. |
| Pedicled Flap | A flap that stays connected to its original blood supply and is tunneled to a new location. |
| Myocutaneous Flap | A flap that includes both skin and muscle. |
| Fasciocutaneous Flap | A flap made of skin, fat, and fascia, but no muscle. |
| Donor Site | The area of the body from which tissue is taken for use in phalloplasty. This can refer to either the flap donor site (where a flap with its own blood supply is harvested) or the graft donor site (where skin is harvested without blood vessels). |
| Recipient Bed | The new location where a graft is placed; provides the blood flow needed for the graft to survive. |
| Primary Closure | Closing a surgical wound directly with sutures, without needing a skin graft. |
| Nerve Ingrowth | A process where nerves gradually grow into a grafted area, which may restore some sensation over time. |
| Split-Thickness Graft | A skin graft that includes the outer layer of skin (epidermis) and part of the dermis. |
| Full-Thickness Graft | A skin graft that includes both the epidermis and the entire dermis layer. |
| Glansplasty | A surgical procedure that shapes the tip of the neophallus to resemble the glans (head) of a penis. |
| Urethral Reconstruction | A procedure to create or lengthen the urethra so urine can pass through the neophallus. |
| Fistula | An abnormal connection or opening between the urethra and the skin. |
| Stricture | A narrowing of the urethra that can block or slow the flow of urine. |
Last updated: 06/20/25