Glansplasty: Aesthetic Refinements of Phalloplasty
Glansplasty, also known as Coronaplasty, is the name of the procedure that constructs the glans penis, which is the bulbous structure at the tip of the penis. In cisgender men, the glans—commonly referred to as the "head of the penis"—is sometimes fully or partially covered by the foreskin, except in those who have been circumcised. The glans penis is anatomically homologous to the clitoral glans.
Glansplasty creates a circumcised-looking penis. The procedure can be done during stage 1, but is sometimes delayed until stage 2 to make sure that there is enough blood supply. (This is especially true with ALT Phalloplasty.) When Glansplasty is performed at stage 2, it can be combined with other procedures. Tattooing the glans for more natural-looking pigmentation is an optional enhancement that is growing in popularity.

Developmental History of Glansplasty
Munawar introduced the first published method of glans
sculpting in 1957. In Munawar's procedure, a circumferential skin
flap about 5mm in width was raised and folded back on itself to
create the coronal ridge. Various techniques emerged after this
but are no longer used.
The most significant development of Glansplasty since Munawar was
the Norfolk technique described in 1988. A circumferential
incision was made in the phallus at a 45-degree angle, about 5 cm
away from the tip on the top of the phallus. Dissection of the
dermal layer was carried out for about 1 cm on the top and down to
0.5 cm on the bottom. This created a skin flap that was folded
inward and sutured. The raw donor surface was then covered with
either a split-thickness skin graft (STSG) or full-thickness skin
graft (FTSG). (Use of a STSG seems to have been standardized as it
creates a more pronounced coronal sulcus compared to a FTSG.)
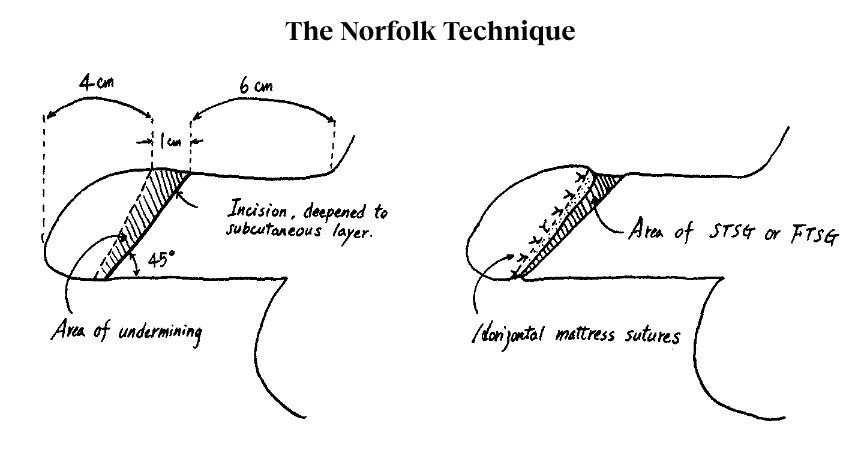
Image source: Fang, R.-H., Kao, Y.-S., Ma, S., & Lin, J.-T. (1998). Glans sculpting in phalloplasty — experiences in female-to-male transsexuals. British Journal of Plastic Surgery, 51(5), 376–379.
 Despite a tendency
for the coronal ridge to flatten out over time, Norfolk became the
most commonly used Glansplasty technique and many surgeons still
use this method, often with their own modifications. For example,
Dr.
Mang Chen, a highly skilled Reconstructive Urologist in San
Francisco, employs a modified Norfolk technique with a
STSG that is harvested from the lower abdomen or groin crease. View
photos of Glansplasty performed by Dr. Chen on his website.
(Note: These photos were taken in the operating room right after
surgery, before any healing has occurred.)
Despite a tendency
for the coronal ridge to flatten out over time, Norfolk became the
most commonly used Glansplasty technique and many surgeons still
use this method, often with their own modifications. For example,
Dr.
Mang Chen, a highly skilled Reconstructive Urologist in San
Francisco, employs a modified Norfolk technique with a
STSG that is harvested from the lower abdomen or groin crease. View
photos of Glansplasty performed by Dr. Chen on his website.
(Note: These photos were taken in the operating room right after
surgery, before any healing has occurred.)
The most recent development in Glansplasty procedures was described by surgeons in Iran in 2019. Like the D'Arpa technique, their method doesn't use a rolled flap. A single medium thickness skin graft is used to cover the area that becomes the coronal sulcus. They found higher patient satisfaction rates with their new method compared to the Norfolk technique. An interesting detail from the procedural description was with regard to the size of the glans, the calculation of which has not been standardized across Glansplasty methods. They determined that glans length was considered equal to phallus diameter.
Ideas for Glansplasty Optimization
To reduce flattening of the coronal ridge, surgeons have explored the use of labial/clitoral hood tissue (Gottlieb), the palmaris longus tendon (Dr. Christopher Salgado, Dr. Jonathan Keith) or a thin strip of acellular dermal matrix inserted into the ridge. Further reconstruction of the ridge can be accomplished with injectable fillers in a revision procedure.
What Is Glansplasty Recovery Like?
If Glansplasty is combined with other procedures, recovery is
dictated more by restrictions required for those procedures. If
Glansplasty is being performed as a standalone procedure,
restrictions will be minimal and you should be able to get back to
non-strenuous activities after a week of rest provided these
activities do not put strain on the skin graft incision.
As always, follow your surgeon's directions for wound management
and restrictions, and contact your surgeon immediately if you see
signs of infection (redness around the incisions that spread,
increased drainage, odour, fever.) Some swelling and bleeding is
expected but if you have concerns, contact your surgeon.
Forgoing Glansplasty for an Uncut Look
Glansplasty is optional. Those seeking Phalloplasty may have cultural, religious or aesthetic reasons for not desiring a circumcised-looking penis and can certainly forgo the procedure. While there is no surgery method available to create foreskin, a tattoo artist experienced with medical tattooing can use color and shading to make a Phalloplasty penis look uncircumcised.
The art of plastic surgery is ever-evolving and further refinement and development of Glansplasty techniques are expected.
References
An
Overview of Female-to-Male Gender-Confirming Surgery
Shane D. Morrison, Mang L. Chen and Curtis N. Crane. Nat Rev Urol
14, 486–500 (2017).
A New Technique for Coronaplasty in Penile
Reconstruction.
Sommeling CE, Wolf EJ, Salim A, Monstrey S, Opsomer D, Claes K,
D'Arpa S. J Sex Med. 2018 Feb 28.
The
Comparison of A New Durable Coronaplasty Technique with Norfolk
Method for Glans Reconstruction after Phalloplasty
Mohammad Reza Akhoondinasab, Mahdy Saboury, Yousef Shafaeei,
Siamak Forghani, and Mohammad Javad Fatemi. World J Plast
Surg. 2020 Jan; 9(1): 39–43.
High
Surgical Complication Rates after Silicone Implant Use for
Improvement of Glans Ridge Appearance
Soumya A. Reddy, B, Curtis N. Crane, MD, Michael Safir, MD, and
Richard A. Santucci, MD, FACS, HON FC Urol. Plast Reconstr Surg
Glob Open. 2022 Jul; 10(7): e4433.
Pelvic
and Urogenical Reconstruction
Jens U. Berli and Richard J. Redett III. Flaps and
Reconstructive Surgery: Flaps and Reconstructive Surgery E-Book,
edited by Fu-Chan Wei and Samir Mardini, Elsevier Health Sciences,
2017, e49.
More Journal articles about Glansplasty »